Women's sexual function is a multifaceted phenomenon that mirrors psychological, physiological, sociocultural, inter- and intra-personal influences, including the health of the whole body and internal systems (Chang et al, 2010; Cunningham et al, 2010; Nunes et al, 2010; Pauleta et al, 2010; Johnson, 2011). Impairments to women's normal sexual function can have negative influences on mental health and quality of life (American Psychiatric Association, 2003; Mercer et al, 2005; Howard, 2010). These problems can also be an economic burden to the family and the healthcare system (Dagher et al, 2012). These burdens are not limited to ‘direct’ diagnostic and treatment costs such as medication, visits to a clinic or hospitalisation, but instead go much further, with ‘hidden costs’ of diseases affecting growth at a macroeconomic level (Trautmann et al, 2016). It has been reported that the cumulative global effect of mental disorders in terms of lost economic output could increase to US $16 trillion in the next 20 years (Bloom et al, 2011).
Pregnancy and childbirth are potentially stressful events for many women and bring many changes to their lives. Women's sexual function is one aspect that can be dramatically affected during and after pregnancy. Sexual problems for women have a prevalence of 25.8%–91% (Khajehei et al, 2009; Echeverry et al, 2010; Ishak et al, 2010; Khajehei et al, 2015; Asselmann et al, 2016). The wide variation in range and prevalence of sexual problems is due to a variety of factors, such as different study populations and research methodologies. In a systematic review of previous studies, it was reported that the mean prevalence of sexual desire disorder, arousal disorder, orgasmic disorder and sexual pain were 64%, 31%, 35% and 26%, respectively (Hayes et al, 2006).
It has been suggested that women's sexuality needs to be considered during the perinatal period, with an emphasis on factors that affect their sexual function and satisfaction (Martínez-Martínez et al, 2017). These factors include, but are not limited to, dyspareunia (Fodstad et al, 2016), breastfeeding (Lagaert et al, 2017), fatigue (Alligood-Percoco et al, 2016), body image (Jawed-Wessel et al, 2016), depression (Khajehei and Doherty, 2017) and relationship dissatisfaction (Khajehei, 2015).
There has been increasing interest in conducting research on the sexual function of women during and after pregnancy. While international studies report a high prevalence of perinatal sexual dysfunction (Echeverry et al, 2010; Ishak et al, 2010; Asselmann et al, 2016), the majority of these studies have adopted a quantitative approach. Quantitative studies emphasise objective measurements and statistical analysis of collected data, but they fail to collect data based on the participants' own words and experiences and fail to reveal underlying ideas through analysing words and phrases (Neuman, 2011). This type of research methodology is possibly premature in an area where authenticated theoretical frameworks are not yet entirely developed (Morof et al, 2003; Barrett et al, 2000; Klein et al, 2009). Unlike quantitative methodology, qualitative research does not deal with numbers. It involves collecting, analysing and interpreting data related to the concepts, experiences and behaviours of individuals (Anderson, 2010). During recent years, there has been a worldwide tendency towards collecting qualitative data on women's sexual function in order to learn from their experiences (Woolhouse et al, 2014; Liu et al, 2013; Martínez-Martínez et al, 2017). Since there are a small number of qualitative studies with up-to-date data from Australia among the literature (Woolhouse et al, 2014), this qualitative study was conducted to obtain women's personal experience of changes in their sexual function during pregnancy and childbirth. It is hoped that these findings will provide a more in-depth understanding and better description of women's personal experiences of pregnancy and childbirth.
Methods
Design
This was a population-based qualitative survey of postpartum women in Australia.
Ethics
This research involved human participants and we received ethical approval from the Human Research Ethics Committee at Curtin University before its commencement. Informed consent was obtained from all individual participants included in the study.
Participants
Postpartum women were invited to participate in this study. Inclusion criteria were that the woman must be between 18 and 40 years old; have given birth to a live baby at 37 weeks or later of pregnancy; have given birth during the past 12 months; be in a relationship with a partner (either heterosexual or homosexual relationship); not be using any antipsychotic medicines; not be pregnant at the time of the study; and must live in Australia.
The National Health and Medical Research Council (NHMRC) guidelines (2007: 19) state that ‘consent should be a voluntary choice’, and because the legal age of consent in Australia is 16 years, women who were 16 years of age or older were invited to voluntarily participate in this study. Women who were older than 40 years were excluded from the study since they were more likely to experience pre- and peri-menopausal changes that have been shown to affect sexual life and mental health (Avis et al, 2009; Hess et al, 2012).
Responses from women were excluded from the study if they met the exclusion criteria of being clinically diagnosed with any psychiatric illness, such as obsessive compulsive disorders (OCD) and anorexia nervosa; or if they were Aboriginal or Torres Strait Islander. This exclusion was based on the National Statement on Ethical Conduct in Human Research (National Health and Medical Research Council, 2007: 69) indicating that ‘researchers should address relevant issues of research design, ethics, culture and language’ if they aim to study Aboriginal and Torres Strait Islander individuals.
Main outcome measures
After a comprehensive literature review, questions were designed to capture data on the topic of pregnancy, childbirth and sexual function (Table 1). A panel of experts, including three sexologists, two midwives and three psychologists, reviewed all aspects of the study and investigated the content validity of the questions. The questionnaire was then reviewed for face and content validity by another 15 researchers who had previously used online questionnaires.
| 1. What makes you most happy (satisfied) in your sexual relationship with your partner? |
| 2. What makes you most unhappy (unsatisfied) in your sexual relationship with your partner? |
| 3. Do you think your last pregnancy affected your sexual function? |
| 4. If your answer to the previous question is ‘yes’, in what way it affected your sexual function? |
| 5. Do you think your last childbirth or delivery affected your sexual function? |
| 6. If your answered ‘yes’ to the previous question, in what way it affected your sexual function? |
| 7. Do you think that your last pregnancy affected your mental health? |
| 8. If your answered ‘yes’ to the previous question, in what way it affected your mental health? |
| 9. Do you think that your last childbirth or delivery affected your mental health? |
| 10. If your answered ‘yes’ to the previous question, in what way it affected your mental health? |
| 11. Do you have any other comments? |
Procedure
After the study received ethics approval, women from across Australia who had given birth in the previous 12 months were invited to take part. An invitation letter containing information about the study and the link to the online questionnaire was posted and distributed on Facebook pages, various search engines, public places and community papers. Snowball sampling also occurred, as participants were asked to pass the website's link onto their friends, family members and relatives who might be interested in participating.
The first two pages of the study website contained information on the research project, including its general purpose, methods and demands, conditions of entry, risks, possible harms and benefits, confidentiality and anonymity, ethics approval, dissemination of the results and consent to participate. Participants were asked to read the information about the study and then provide consent by ticking the ‘consent to participate’ box if they agreed to participate. Since this was an anonymous study, the participants were asked not to provide their names or contact details. Participants were then directed to the next pages to answer the questions.
Data considered for inclusion and exclusion were derived from responses to the questions seeking information on the woman's age, country of residence, ethnicity, relationship status, pregnancy, the gestational age at birth of their last child, age of the child and presence of a mental health condition. These criteria were clearly listed on the study website before the participants answered any questions. Women who were not eligible were requested not to participate by an instant screen message. Despite this, some women chose to answer the study questions. Therefore, at the time of data analysis a total of 128 women were excluded: 67 of whom lived in other countries; 12 of whom were of Aboriginal or Torres Strait Islander background; 8 who were not in a relationship; 5 who were pregnant; 8 who had given birth before the 37th week of pregnancy and 28 who reported mental health problems such as OCD, anxiety, phobia and post-traumatic stress disorder (PTSD). The online questionnaire was available for four months from May–August 2012.
Data analysis
Providing responses to the questions was not mandatory because the researchers assumed that creating and inputting responses might have added a burden for some women, especially those who experienced undiagnosed or undeclared mental health issues or postpartum depression. As a result, a different number of participants responded to each question. Table 2 shows a summary of the responses given to each question. More than one-third of the women (35%) reported that their last pregnancy affected their sexual function, 33% experienced changes in their sexual function after childbirth, 24% reported changes in their mental health during pregnancy and 26% had their mental health affected by childbirth. Women who reported not being affected by pregnancy and childbirth (answered ‘No’ to questions 3, 5, 7 and 9), either did not provide additional information, or mentioned that they had not resumed sexual activity after childbirth. The themes were then explored among the responses from women who answered ‘Yes’ to those questions and provided further details. Some women typed a few sentences and a few women wrote up to two pages. The average response length was one paragraph.
| Responses | ||
|---|---|---|
| Questions | Yes n (%) | No n (%) |
| Do you think your last pregnancy affected your sexual function? (n=273) | 114 (35%) | 159 (49%) |
| Do you think that your last pregnancy affected your mental health? (n=267) | 79 (24%) | 188 (58%) |
| Do you think your last childbirth or delivery affected your sexual function? (n=265) | 106 (33%) | 159 (49%) |
| Do you think that your last childbirth or delivery affected your mental health? (n=266) | 84 (26%) | 182 (56%) |
Data were analysed using Colaizzi's (1978a; 1978b) process for thematic analysis. All participants' descriptions of the changes in their sexual function during pregnancy and after birth were read, reviewed, coded and assigned to major, broad categories, which were identified by different colours. Next, important statements that related directly to the changes in sexual function were extracted, to help formulate definitions for these important statements, which were then categorised into clusters of themes. During this process, each reviewer conducted an inductive analysis that resulted in emergence of the descriptive themes to answer the research questions. Each reviewer first did this independently and then as a group. Through group discussions, more analytical themes emerged. This cyclical process was repeated until the new themes were sufficiently described and all initial descriptive themes were explained. Integrating the findings into a comprehensive description of the changes in women's sexual function during pregnancy and after birth was the next step. Finally, modifications were incorporated into the final description of the changes in women's sexual function. The emergence of patterns resulted in a more sophisticated level of coding, which assisted the development of sub-themes and conclusions.
Results
Of the participants, 52% were aged 21-30 years old, 67% had a university degree, 51% had no formal occupation, 69% had annual income of ≥50 000 AUD and 73% were multiparous (Table 3).
| Characteristic | n (%) |
|---|---|
| Age (years) | |
| 18–20 | 13 (5%) |
| 21–30 | 143 (52%) |
| 31–40 | 117 (43%) |
| Education | |
| Diploma or lower | 90 (33%) |
| University degree | 184 (67%) |
| Career | |
| No formal occupation | 138 (51%) |
| Formal occupation | 135 (49%) |
| Annual income of family (AUD) | |
| ≤ $50 000 | 84 (31%) |
| ≥ $50 000 | 189 (69%) |
| Ethnicity | |
| Oceanian (Australia and New Zealand) | 128 (47%) |
| American | 63 (23%) |
| European | 52 (19%) |
| African and Middle Eastern | 16 (6%) |
| Asian | 16 (6%) |
| Parity | |
| Primiparous | 74 (27%) |
| Multiparous | 199 (73%) |
The data generated five main themes and several sub-themes (Figure 1). The themes were: mental health changes, obstetric violence, relationship issues, physical changes and role conflict. The contents of each theme and its sub-themes are described below and explained using quotes from the participants.
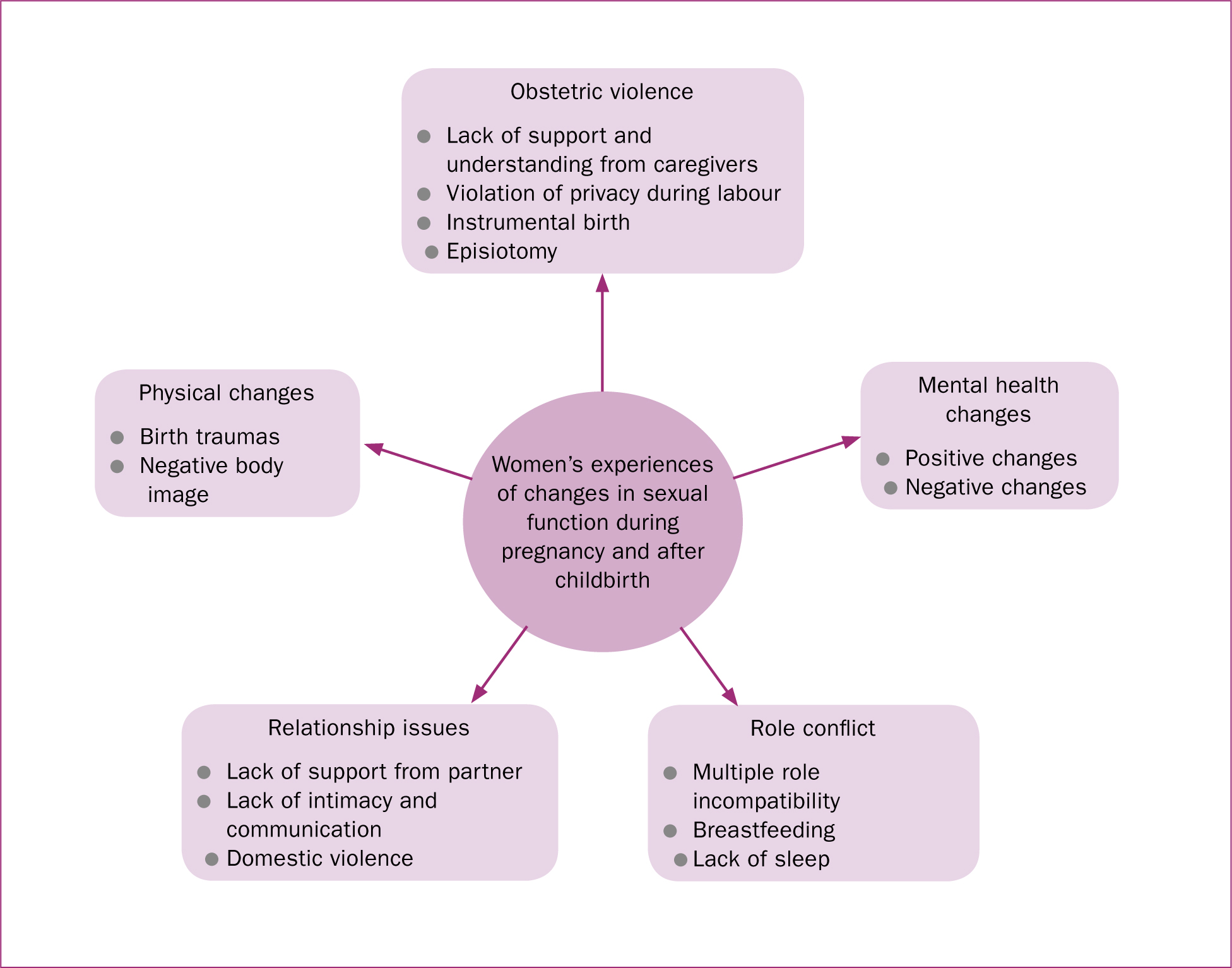
Mental health changes
Mental health changes had two main sub-themes: positive changes and negative changes. The positive changes in mental health and sexual function during pregnancy and after childbirth were reported to be due to role transition, new responsibilities and feeling empowered, confident, happier, a better person, more relaxed and centred, clearer in mind and more mature after going through the process of labour and birth. For example, one woman said:
‘It [childbirth] made me happier. I felt more loved and in love with my husband. This caused my mind to be at ease and for me to relax.’
Another woman commented:
‘I feel more confident in myself and my sexuality. I felt very empowered in my childbirth. And when I go through tough times in motherhood I look at the situation and say if I overcame and conquered in birth then I can overcome and conquer in anything that comes my way.’
On the other hand, the mental health of some women (n=37) was negatively affected by factors such as the experience of birth, hormonal fluctuation, brain–body disconnection, difficult emotions, depression, fears and stress, violation of privacy during labour and lack of confidence. These negative changes had a negative impact on the women's sexual function, which made the women concerned for when their sexual function would return to normal. For example, one woman commented:
‘Childbirth seems to have completely removed my libido! It's like the hormones are not there! I want to have sex, but not because I feel like having sex. I just want to be close to my husband and be with him in that way, I just wish my body was into it. I don't get turned on at all … I'm not used to having no libido and I'm scared it will never come back.’
Another woman said:
‘To me it feels like there is a broken connection between my brain and my vagina! … I find it hard to get aroused and in the mood for sex … I also find it very hard to orgasm now.’
Obstetric violence
Obstetric violence was described by respondents as neglected needs and wishes, verbal humiliation, invasive practices and forced medical intervention. These, in turn, resulted in the violation of women's right to make voluntary choice and have reproductive autonomy during pregnancy, childbirth and the postpartum period. Subthemes of obstetric violence were shown to be: lack of support and understanding from caregivers, violation of privacy during labour, instrumental delivery and episiotomy that evoked an image of rape. One woman mentioned that:
‘It left me feeling like a failure, a sexless eunuch, not a true woman … The birth rape, the lack of support from hospital staff and family.’
Another woman said:
‘I was pretty traumatised by the actions of my caregivers in the last hour of my birth. I was forced to push on my back, I was forced to ‘purple push’, I was cut without being asked for consent. My daughter was born via vacuum, the feeling of her literally being dragged out of me while a team of people held me down was horrific. The episiotomy took months to come together, I had swelling for almost a year. I had pelvic pain for months after giving birth. Whenever I tried to talk about these things I was chastised and told that I should be thankful for a healthy baby. I don't see how the two are related … I am traumatised by the actions of my caregivers. There is a total lack of support when it comes to helping women process their birth experiences.’
Another woman complained that the issue was taken for granted and not talked about by clinicians:
‘I think everyone seriously underestimates the changes that will happen to your mind and body after being pregnant. Everyone talks about during the pregnancy and straight after but nothing about months and years down the track how it can really change your body so much.’
Relationship issues
The theme of ‘relationship issues’ contained other subthemes, including lack of support from partners, lack of intimacy and communication, and domestic violence.
Lack of support from their partner after birth was reported to cause sexual problems. One woman mentioned that:
‘My husband works away so he is only home once a month or so and wants to get his ‘quota’ in before he leaves again.’
Some women (n=24) reported that their sexual problems were due to the lack of emotion in their relationships during pregnancy and after childbirth. They were dissatisfied that their partners considered only the physical aspect of sex and ignored their needs for intimacy and closeness. They reported that they felt pressured into being a receptacle for their partners' needs. For example, one woman said that she was affected by:
‘The lack of remembering by my partner that a woman is all about the entire body, not just the vagina.’
Other women commented that:
‘He counts quantity over quality … I do wish he would want to spend time not just having sex but intimacy, romance, cuddling as well.’
Lack of communication with the partner accompanied by mismatched libido caused sexual problems. Some women (n=8) reported they wanted their partners to initiate sex more often, while others (n=23) reported sexual dissatisfaction due to their partners being absent from home, having long working hours, nagging, expressing a lack of interest, or having an affair.
For example, one woman mentioned:
‘Pain during and after intercourse due to anxiety around my partner looking elsewhere for sexual intimacy … he turned to pornography, and because he wasn't working it was more often than I would [have] liked, so that was degrading.’
Violence and abuse within the relationship, and not receiving enough support from the community were noted as other factors that caused sexual problems among the participants. For example, one woman stated:
‘Domestic abuse [is a] big factor for many women and sex is affected. My partner became borderline abusive, verbally and [was] throwing things with terrible scary threats … left me with no desire for sex … very little help given, [clinicians'] response is only to study us more and make us fearful of them.’
Physical changes
Physical changes was another major theme, which could be divided into sub-themes including birth traumas and negative body image. Birth trauma caused by different modes of birth was reported to cause physical changes and affect women's sexual function. For some women (n=18), caesarean section was a negative event that affected their sexual function. One woman, who had given birth by caesarean, said that:
‘Following my caesarean delivery, my lower abdomen between my pubic bone and navel were completely numb and flaccid for 8 months … I feel that the numbness in my lower abdomen extends somewhat below the pubic bone, deadening my clitoral sensation which makes it difficult to orgasm.’
Others (n=22), however, reported that their sexual problems, lack of desire, painful intercourse and lack of orgasm were due to a traumatic vaginal birth, particularly if their baby was reported to be large. A few women (n=7) reported that birth trauma resulted in urinary incontinence and this has made them self-conscious during sex, saying, that giving birth to a larger baby was:
‘A very traumatic birth … do not feel the same. It is very tight inside and penetration feels like the skin is stretching … I think I may have urinated once during orgasm because my muscles aren't as strong.’
Negative body image was reported by the women as another factor that they felt contributed to their sexual dissatisfaction. Some women (n=13) did not feel comfortable with the physical changes that had taken place and reported a lack of confidence in their body due to weight gain and changes during pregnancy and after birth. As one woman commented:
‘I don't feel sexy anymore; I feel fat and I am not satisfied with my physical appearance at all.’
Another woman stated:
‘Confidence! That I would still be enough for my husband and not stretched beyond all recognition! … Less confidence around the rest of body.’
Role conflict
Adapting to the new motherhood role was a further major theme identified in this study, and could be divided into subthemes that included the incompatibility of multiple roles, the challenges of breastfeeding, and a lack of sleep. As reported by the women, childbirth meant less sleep, less free time and more fatigue. Consequently, instead of having sex, women wanted to sleep or have time for themselves, and that led to a changed sex pattern. For example, one woman mentioned that it was:
‘Hard to separate being a mum, being a wife and still being me … I also just don't feel like myself anymore.’
Another woman said that she felt:
‘Like everyone wants a part of you. No time on your own. Go to bed you rest from kids but feel like you need to be there for hubby then … I feel depleted and tired yet I can't sleep … no energy for sex.’
Some women who breastfed (n=19), reported that sharing a bed with the baby resulted in an unsatisfactory sex life, as they were concerned about accidentally waking or harming the baby. Other breastfeeding women reported that their sexual activity was negatively affected by both breastfeeding and having a toddler at home. For example, one woman said:
‘We bed-share with our son. Plus, he's a poor sleeper and that the baby and toddler seem to always wake up when we try to have sex! It definitely has a negative impact on our sex-life.’
Discussion
In this study, 273 women were recruited through an online survey to investigate the changes in their sexual function during pregnancy and the first year after childbirth. Five main themes were identified: mental health changes, obstetric violence, relationship issues, physical changes and role conflict.
Some women found that pregnancy and giving birth helped them to gain a new perspective and improved their sexual function by making them feel empowered and relaxed. These findings support previous research (Ngai et al, 2011) indicating that childbirth-induced changes were considered to be empowering and could contribute to improved sexual function.
Other women reported that pregnancy and childbirth had negative effects on their sexual function. Adapting to their new roles as parents, taking care of the newborn, tiredness, lack of sleep and less free time were mentioned, which meant that mothers preferred to sleep or look after themselves in their limited free time. This reportedly conflicted at times with the partner's sexual desire, with negative consequences on their sexual life, a finding that corroborated previous research (Olsson et al, 2005). Indeed, becoming a mother, a mismatch between expectations and realities of motherhood, women's attitudes to pregnancy, birth-related changes and the ability to adapt to new responsibilities may play a significant role in negative experiences of pregnancy and childbirth (Amankwaa, 2003; Luyben et al, 2011; Ngai et al, 2011). It has been reported that being a mother makes many women ‘feel isolated, alone and depleted rather than nurtured and supported’ (Barclay et al, 1997: 727; Olsson et al, 2005; Williamson et al, 2008; Zuriati, 2017).
An Australian study by Williamson et al (2008) reported that pregnancy and childbirth affected the sexual function of the many couples who participated in the study and negatively influenced their relationships. Feeding the baby at night, perineal tears, tiredness, dedicating more time to the baby and less time to the partner, and loss of sexual desire were mentioned as factors that interfered with couples' sexual lives and relationships. In that study, only one couple declared that their sexual desire and activity increased after childbirth and their relationship became stronger, as they had abstained from sex during pregnancy due to the fear of hurting the baby and they looked forward to resuming sex after birth. Similar results were also shown in a study by Muise et al (2017). These reports agree with the findings of our study, indicating that interpersonal issues, birth-related trauma and the need to care for the baby affect the sexual function of women after birth.
The women in this study stated that they needed to be assured of being loved and appreciated outside the bedroom. The women reported wanting their life with their partner to be their focus, not just their sex life, especially as women need to connect emotionally, mentally and intellectually before they can connect sexually (Ramsey and Hoyt, 2015). Earlier literature has shown that women have an inclination towards keeping sex and love separate and that emotional connection and being loved are the determinants of a satisfactory intimate relationship for many women (Basson, 2000; Brotto et al, 2008; Schoenfeld et al, 2017).
Obstetric violence, another theme that was discovered in this study, is a frequently disregarded type of violence against women in maternity care. Performing an episiotomy without woman's consent, being held down during birth, extracting the baby from the mother's body, and having a caesarean section while the threat of vaginal birth (if any) to the baby or mother was not communicated or made obvious (or when a caesarean contradicted their birth plans) were examples of obstetric violence reported by participants. These discriminations and violation of women's rights and privacy are not limited to these cases and can happen anytime during pregnancy, childbirth and postpartum period (Pérez D'Gregorio, 2010). Research has shown that mistreatments such as verbal humiliations, physical violence and forced medical interventions can result in degrading childbirth, postpartum health complications and severe psychological trauma. According to the World Health Organisation (WHO) (2017), violence and discrimination that occurs during birth may not be documented in medical notes or may not be reported by the women due to fear and shame. WHO recommends providing support for further research on defining and measuring obstetric violence worldwide in order to better recognise its effects on women's health experiences and choices (WHO, 2017).
Despite the significance of the issue, most women choose not to discuss obstetric violence during routine antenatal and postpartum visits because of factors such as embarrassment, lack of trust, or fear of a lack of empathy from clinicians (Khajehei et al, 2015). Health professionals have also been shown to be reluctant to talk about these issues due to potential barriers such as cultural factors, embarrassment, lack of knowledge and time limitations (Pauleta et al, 2010). The information obtained from this study can help shape future interventions and enhance knowledge and awareness of the problems among nurses, midwives and other health professionals.
Sexual health education has been shown to promote women's sexual and marital satisfaction and improve their quality of life (Mahmodi and Valiee, 2016). Educational sessions can be held to inform pregnant or postpartum women and their partners about changes in sexual function, mental health and the quality of relationships, while providing information on adapting to their new roles and responsibilities during and after pregnancy. Training should include strategies for providing active, woman-centred counselling with an open atmosphere to enable postnatal women to freely discuss their issues, needs and expectations (Edvardsson et al, 2011), to help women pursue more effective coping strategies. Peer support groups can also provide postnatal women with support and guidance to help them find answers to their questions, resolve their problems and increase involvement in community activities (Doornbos et al, 2013). Providing timely and appropriate professional counselling and support can help women maintain a good quality of life.
‘Some women in the study found that pregnancy and giving birth helped them to gain a new perspective of themselves and improved their sexual function by making them feel empowered and relaxed’
Implications for practice
Primary care services and health professionals should consider how the sexual function of women may change during and after pregnancy, with an integrated approach to improve their overall wellness (Wincze and Weisberg, 2015). Assessment of sexual function needs to be included in perinatal visits, where appropriate and timely education, counselling and support should be provided. Health professionals should initiate conversations in a confidential and friendly environment, asking open questions and shaping the dialogue so that the women feel comfortable to express their concerns and seek support (Bahadoran et al, 2015; Rivas et al, 2016). To address obstetric violence, appropriate education and training are required to enhance awareness, improve interactions, promote respectful practice and enhance the quality of services provided (Sadler et al, 2016).
Limitations and strengths
Similar to other studies, the present study has some limitations. First, the online nature of the questionnaire excluded women who were not computer literate or had no access to a computer. The study also relied on self-reported data, which has inherent limitations. However, as the study was anonymous, with no face-to-face contact, it is reasonable to conclude that the participants provided honest, trustworthy responses. Furthermore, because participants were not selected randomly across Australia, women with negative experiences might have been over-represented and women who reported symptoms of depression might have been under-represented due to a selection bias. Thus, the results obtained from this study cannot be generalised to the entire population of postpartum women in Australia, but can operate as an informative aspect within the greater body of knowledge.
Despite these shortcomings, it is fair to conclude that the present study offers important contributions to the literature and supports the case for future studies in this context. The primary strength of this study is its use of online questions and anonymous participation. This allowed the women to feel free to express their thoughts and to provide honest responses. Women could also visit the study website and respond whenever they had time, which may also have contributed to the high response rate to each question.
Further research is needed to randomly select postpartum women and explore the impact of pregnancy and childbirth on women's sexual function, mental health and relationships. Further in-depth interviews are required to refine the nature of questions asked in this study and shape a detailed dialogue, in order to investigate how pregnancy and postpartum changes influence women's sexual function, relationship satisfaction and mental health.
Conclusion
Five main themes were discovered in this study: mental health changes, obstetric violence, relationship issues, physical changes and role conflict. While some women experienced no changes in their sexual function during pregnancy and after childbirth, others reported some negative impacts of pregnancy and childbirth on their sexual function, while some women reported that their sex lives improved during pregnancy or after giving birth.
This indicates that pregnancy and childbirth cannot necessarily be negative experiences. Pregnancy and giving birth can help women feel empowered and relaxed and have better sexual function. To achieve this, women need to be assured of being loved and appreciated outside the bedroom and need to connect emotionally, mentally and intellectually before they can connect sexually.

